Blood sugar can be controlled by weight loss, not surgery: WUSTL experts
Gastric bypass surgery has been thought to offer advantages, independent of weight loss, for improving insulin sensitivity and blood glucose levels in obese patients. But new research at Washington University School of Medicine in St. Louis shows that those improvements are related to weight loss alone and not to the surgical procedure itself.
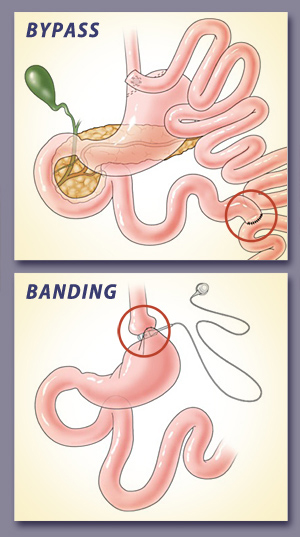
Gastric bypass (top) reduces the size of the stomach and re-routes food to lower in the intestine. Gastric banding (below) places a ring around the upper portion of the stomach to make it smaller.
In a study comparing gastric bypass to laparoscopic adjustable gastric banding, the researchers report that although both procedures help patients lose weight, gastric bypass does not provide additional advantages for improving the secretion of insulin or the body’s sensitivity to insulin in obese patients who don’t have diabetes. The study is available online in the Journal of Clinical Investigation.
“It’s been proposed that surgically diverting food from the upper intestine, as occurs in gastric bypass surgery, improves blood glucose control and insulin sensitivity in obese patients independent of weight loss,” says senior investigator Samuel Klein, MD. “But when we did careful evaluations after patients lost the same amount of weight with either surgery, we found that the improvement in the secretion of insulin and the ability to dispose of glucose in response to insulin were identical in both surgical groups.”
Klein, the Danforth Professor of Medicine and Nutritional Science, directs the Division of Geriatrics and Nutritional Science and the Center for Applied Research Studies as well as Washington University’s Center for Human Nutrition. His team gathered data from 20 patients at Barnes-Jewish Hospital in St. Louis. Half had gastric bypass surgery and half had adjustable gastric banding.
The researchers measured the ability of the pancreas to secrete insulin after a meal. They also evaluated the ability of muscle tissue to metabolize blood glucose in response to insulin before surgery and again after patients lost 20 percent of their body weight. All of the people in the study had been extremely obese before surgery, but none had type 2 diabetes.
“We purposely did not enroll people with diabetes in this study to eliminate the influence of diabetes medications and differences in blood sugar control before surgery on our outcome measures,” Klein says. “But we are currently studying the effects of bariatric surgery in patients with type 2 diabetes, to see whether there is any difference between surgical procedures in the regulation of glucose control in this patient population.”
Bariatric surgery, such as gastric bypass and gastric banding, helps patients rapidly lose weight and often brings type 2 diabetes under control.
Gastric bypass reduces the size of the stomach by more than 90 percent and re-routes food lower in the intestine. Gastric banding places an inflatable ring around the upper portion of the stomach, making it smaller.
“Bariatric surgery is the most effective therapy we have for treating obesity and type 2 diabetes,” he says. “Patients who have gastric bypass tend to lose more weight than those who get gastric banding. The difference in weight loss between the two procedures is a major reason for choosing bypass over banding. But in this study, we compared patients after the same amount of weight loss to make sure differences in the amount of lost weight would not affect our results.”
The bypass patients also experienced rapid absorption of glucose after a meal, causing more insulin to be produced. Klein says that seems to be a unique metabolic feature in gastric bypass patients, and the clinical effects of the spikes in glucose and insulin are not clear. What is clear, he adds, is that weight loss following both types of surgery improves metabolic health.
“Not only does insulin sensitivity improve, but the cells that secrete insulin work better,” he says. “There were dramatic improvements in both surgical groups, so it appears that losing weight is the primary factor responsible for reversing the abnormalities in insulin secretion and glucose metabolism that are associated with obesity.”
Bradley D, Conte C, Mittendorfer B, Eagon C, Varela JE, Fabbrini E, Gastaldelli A, Chambers KT, Su X, Okunade A, Patterson BW, Klein S. Effects of gastric bypass and adjustable gastric banding on glucose homeostasis. Journal of Clinical Investigation vol. 112, published online Nov. 26, 2012 http://www.jci.org/articles/view/64895?key=31c84cf8f52f834d9914
Funding for this research comes from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the National Center for Research Resources of the National Institutes of Health (NIH). Additional funding was provided by a grant from Ethicon Endo-Surgery and the Atkins Foundation Philanthropic Trust. NIH grant numbers DK37948, DK56341, UL1 RR024992 and RR00954.
Samuel Klein serves on a scientific advisory board for Ethicon Endo-Surgery.

No comments:
Post a Comment